Talk therapy is best for some people; antidepressants are better for others. Scientists say PET scans might help figure out early on what treatment a person needs.
iStockphoto.com
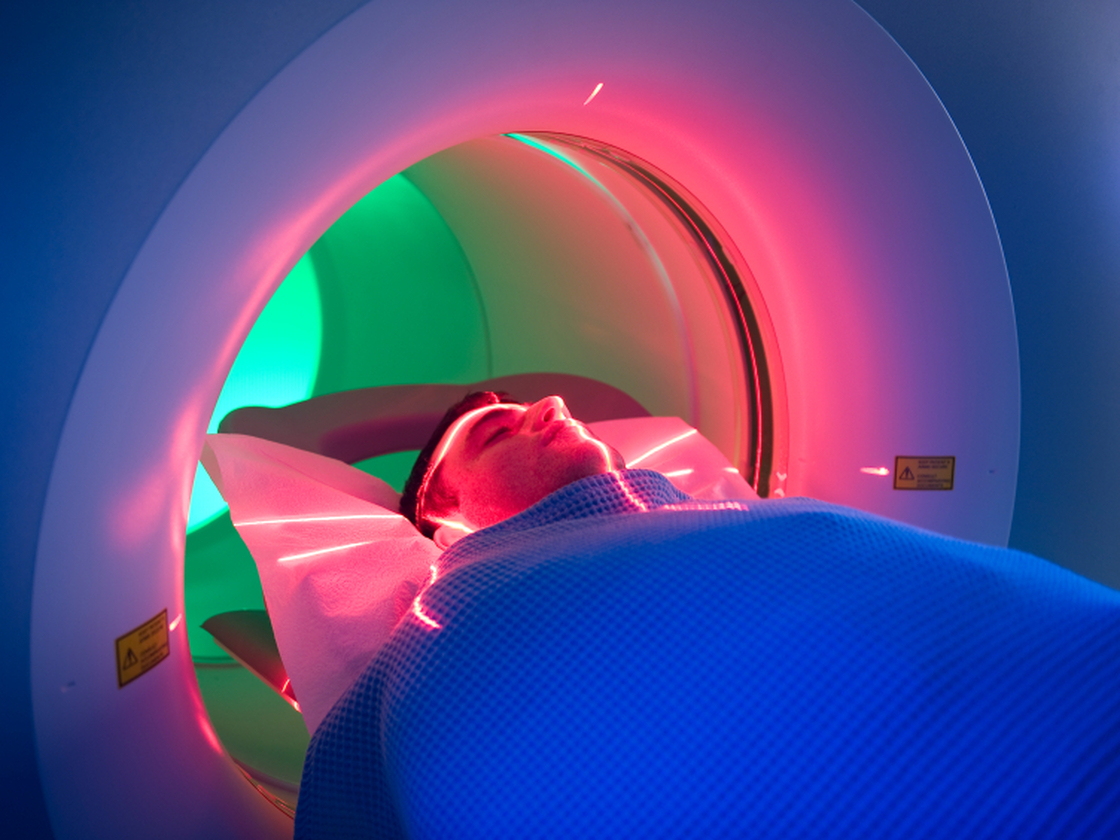
Talk therapy is best for some people; antidepressants are better for others. Scientists say PET scans might help figure out early on what treatment a person needs.
iStockphoto.com
Finding the right treatment for depression can be a struggle. People find relief with the first treatment only 40 percent of the time. Trying different antidepressants or therapies can take months, which means months of suffering.
Scientists are trying to better the odds by searching for signals in the body or in behavior that could be signposts to the right treatment. Researchers at Emory University say that PET scans of the brain may help predict which people do better on SSRI antidepressants, and which would benefit most from cognitive behavioral therapy instead.
They scanned the brains of 65 people with depression, then assigned them to get either 12 weeks of treatment with an antidepressant or 12 weeks of cognitive behavioral therapy. Just 38 people had clear responses to either treatment at that point. Twelve did well with talk therapy, while nine failed to improve. Eleven did well with the antidepressant, while six had no improvement.
Then the researchers took those results and matched them up with the earlier PET scans, which reflected activity levels in different parts of the brain. The people who did well with therapy had less brain activity in the insula, a brain region that's involved in emotion and self-awareness. The people who did well with medication had a more active insula.
The authors of the study, which was published online in JAMA Psychiatry, readily acknowledge that this concept has a long way to go to become a reliable, practical medical test.
"I put this study in the category of intriguing but extremely preliminary, and certainly not something that clinicians can begin to use as they're making treatment decisions," says Dr. Daniel Carlat, an associate clinical professor of pyschiatry at Tufts Medical School, who was not involved in the study. He thinks it would take 10 to 15 years of further research to make it useful in medical practice.
Other researchers have used PET scans to predict which antidepressant would work for individuals. But so far no one has done studies that are big enough to prove their utility for medical tests.
Scientists are widening the hunt for biomarkers that could guide depression treatment, much as tests are used to guide treatment for cancer and heart disease.
The ideal biomarker for depression treatment would be simple and inexpensive, along the lines of a blood test or EEG. A PET scan is probably not that test.
PET scans are expensive; Medicare pays about $1,100 for a head scan, and retail prices are higher. Patients have to be injected with radioactive tracer liquids that often have to be made in a cyclotron, so they're not something you'll find in a doctor's office, or even every hospital. (Earlier this year, Medicare refused to pay for PET scans for diagnosing Alzheimer's.)
So researchers are looking at other possibilities, including different types of brain scans that measure brain function and structure; EEGs, which measure the brain's electrical activity; and blood flow in the brain.
Looking beyond the brain, they're also looking in the blood for differences in proteins, immune factors, growth factors, and genes. Then there are behavioral and cognitive tests, which measure a person's thinking, reaction time, and memory.
The ideal would be to have the depression equivalent of the Framingham risk profiles for heart disease, which evaluates a person's risk of heart attack by looking at many different factors.
That's what Dr. Madhukar Trivedi hopes to come up with for depression. He's a professor of psychiatry at University of Texas Southwestern Medical Center, and leader of the EMBARC clinical trial, which is in the midst of testing the validity of a wide variety of markers for depression on 400 people.
Cheaper, simpler tests — the equivalent of a cholesterol test — might be used for initial screening when someone first is diagnosed, Trivedi speculates. More complex, expensive tests like PET scans might be reserved for people who have tried various treatments and found that none worked.
"The place you might get [health insurers] to pay for it is in treatment-resistant depression," says Dr. Daniel Silverman, head of neuronuclear imaging at the UCLA Medical Center. The cost of medications for a year of failed treatments is more than the cost of a PET scan, he notes, and it might save people from "months and months of pain."


